BICEPS – TENDINITIS
Click on Image to Enlarge
- TENDINOPATHY: is typically used to describe any problem involving a tendon. The tendons can be worn, injured, stretched, and/or torn.
- TENDONITIS: Once used to describe almost any tendon pain, medical professionals now only use the term tendonitis to describe acute inflammation of the tendon due to small (micro) tears (the suffix “itis” indicates inflammation)
- TENDINOSIS: is the non-inflammatory degeneration of a tendon. This degeneration can include changes to the structure or composition of the tendon. These changes often result from repetitive strain-injuries to a tendon without adequate time to heal.
| COMPARISON FACTOR | TENDONITIS | TENDINOSIS |
|---|---|---|
| Recovery time in acute cases | 2 to 3 days | 2 to 3 months |
| Recovery time in chronic cases | 4 to 6 weeks | 3 to 6 months |
| Long-term outlook with non-surgical treatment | Almost 99% of cases recover completely | Up to 80% of cases recover completely |
| Treatment goals | Decrease inflammation by: Rest, anti-inflammatory medication (short-term course), icing the tendon intermittently, and/or use of cast or splint | Encourage formation of collagen and other proteins by: Physical therapy, exercise, and/or surgery (in some cases) |
| Long-term outlook after surgery | Almost 95% of cases recover after surgery | 70 to 85% of cases recover after surgery |
| Recovery time after surgery | 3 to 4 weeks | 4 to 6 months |
SOURCE: SPORTS-HEALTH.COM
What is Biceps Tendinitis?  – Healthy Street
– Healthy Street
Overview
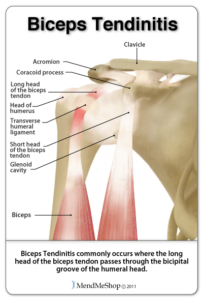
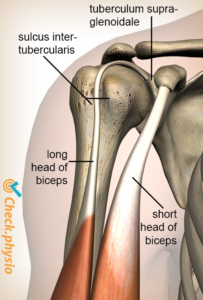
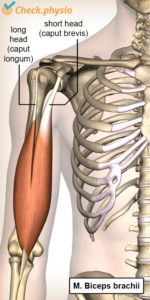
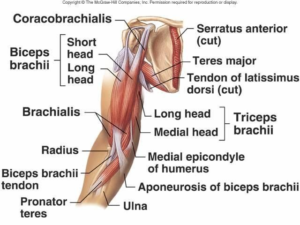
– The biceps muscle has two heads, simply named the long head and the short head.
– With biceps tendinitis, it’s usually the long head (which attaches to the top front of the shoulder) that gets injured.
– The long head tendon attaches to the shoulder joint capsule
Injury
– When the biceps tendon has any kind of abnormal or excessive stress, it may get inflamed.
– This includes excessive tension (pulling), compression (pinching), or shearing.
– If this happens repetitively, your body’s ability to heal itself may lag compared to these stresses, and this can lead to pain and injury via inflammation and swelling
Risk Factors for Biceps Tendonitis
1. Repetitive overhead movements.
2. Poor movement mechanics and posture.
3. Weakness in the rotator cuff.
4. Age-related changes.
5. Abrupt increase in upper body exercise routine
How Do You Know If You Have Biceps Tendonitis?
– People often have a deep ache in the front of the shoulder; pain is usually localized at the bicipital groove.
– Sometimes pain can radiate distally down the arm. Symptoms will usually come on with overhead motions, pulling, lifting, or the follow-through of a throwing motion.
– Instability of the shoulder may also present as a palpable or audible snap when shoulder motion occurs
Common Symptoms of Biceps Tendonitis
1. Sharp pain in the front of your shoulder when you reach overhead.
2. Tenderness to touch at the front of your shoulder.
3. Dull, achy pain at the front of the shoulder, especially following activity.
4. Weakness felt around the shoulder joint, usually experienced when lifting or carrying objects, or reaching overhead.
5. A sensation of “catching” or “clicking” in the front of the shoulder with movement.
6. Pain when throwing a ball.
7. Difficulty with daily activities, such as reaching behind your back to tuck in your shirt, or putting dishes away in an overhead cabinet.
Treatment Plan
– Manual therapy is great to loosen tight muscles, mobilize stiff joints, and improve the blood flow in target areas.
- Step 1: Reduce Inflammation
– Rest and cold compress will help to reduce inflammation and begin the healing process. - Step 2: Range of Motion
– Once the pain has begun to subside, you should start to work on improving your pain-free range of motion.
– This will include not only the glenohumeral joint but also the neck, trunk and scapula
– If you have adequate flexibility in all of these other parts of your body, your glenohumeral joint won’t have to work as hard.
– Two important ranges of motion for the shoulder include: flexion and internal rotation. You should be able to reach all the way overhead (full flexion) and have full internal rotation without pain.
– Having tight muscles in the back of your shoulder can lead to increased stress at the front of your shoulder, right where your biceps tendon is. - Step 3: Build Strength
– Early in your recovery, you can work on pain-free strengthening of the muscles in the shoulder as well as the back muscles that support the shoulder.
– The rotator cuff muscles help to stabilize and protect the glenohumeral joint, so any basic shoulder-conditioning program should begin with these.
– You also want to focus on stabilizing your scapula, which is the base that the humerus moves on. The shoulder girdle must be strong and stable enough to transfer all the forces between your arm and your body, and it must also be mobile enough to move with the humerus to allow for full range of motion. - Step 4: Functional Training
– Once you’ve started the healing process, significantly decreased inflammation, gained full range of motion, and have started strengthening, you’re ready for functional training.
– This is the last and most rewarding part of rehab because you’re now training to regain full strength and function.
– You move with your entire body in a coordinated fashion, whether you want to return to playing baseball or carry a basket of laundry.
– If you move improperly (PTs refer to this as aberrant motion), this places increased stress to your tissues, which can lead to damage over time.
– So, even if your diagnosis is biceps tendonitis, a good physical therapist will know to treat the entire body.
– Whatever your goal is after physical therapy, your treatment should teach you to move more efficiently and optimally prepare you to return to your normal life.